Scientists have identified a persistent change in a handful of blood proteins in people with long Covid that indicates that an important part of their immune system remains on high alert for months after an acute infection.
The findings, published Thursday in the journal Science, could help explain what causes the persistent fatigue, brain fog and other debilitating symptoms of long Covid, as well as pave the way for diagnostic tests and potentially, a long-awaited treatment, experts say.
The study followed 113 Covid patients for up to one year after they were first infected, along with 39 healthy controls. At the six-month mark, 40 patients had developed long Covid symptoms.
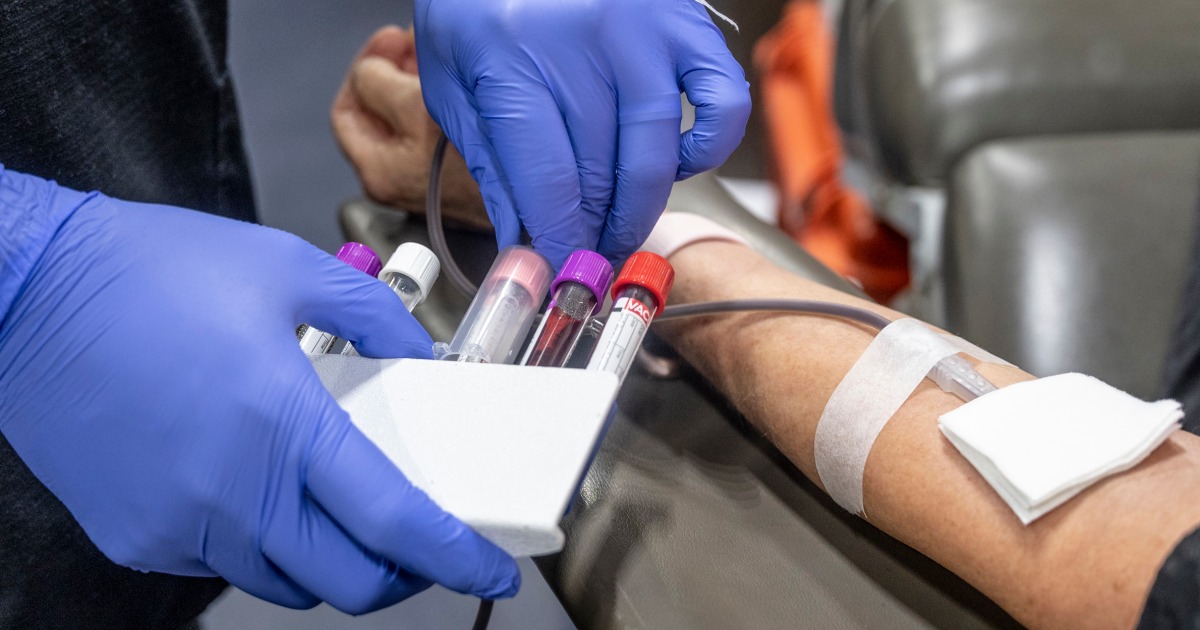
Repeated blood samples turned up important differences in their blood: A group of proteins indicated that a part of the body’s immune system called the complement system remained activated long after it should have returned to normal.
“When you have a viral or bacterial infection, the complement system becomes activated and binds to these viruses and bacteria and then eliminates them,” said Dr. Onur Boyman, a professor of immunology at the University of Zurich in Switzerland and one of the study’s investigators. The system then returns to its resting state, where its regular job is to clear the body of dead cells, he said.
But if the complement system remains in its microbe-fighting state after the viruses and bacteria are eliminated, “it starts damaging healthy cells,” he said.
“These can be endothelial cells that line the inner layers of blood vessels, the cells of the blood itself, and cells in different organs, like the brain or the lungs,” he continued. The result is tissue damage and microclots in the blood.
Previous studies have documented blood clotting and tissue damage in people with long Covid. “But this research gets at the molecular mechanism of how that might be initiated,” said Akiko Iwasaki, a professor of immunobiology and molecular, cellular and developmental biology at the Yale School of Medicine, who was not involved with the new study.
Tissue damage along with blood clots can lead to the disabling symptoms of long Covid, including an intolerance to exercise.
During exercise, the heart pumps more blood and agitates the endothelial cells inside blood vessels, which are everywhere in the body, Boyman said.
“In healthy people, normal endothelial cells can take these changes, but the inflamed endothelial cells in long Covid patients cannot,” he said.
Iwasaki noted that microclots can reduce the level of oxygen and nutrients delivered to different organs.
“If your brain, for example, isn’t getting enough oxygen, obviously there will be a lot of issues with memory, brain fog and fatigue,” she said.
A possible path to tests and treatments
A little more than 14% of adults in the United States report ever having experienced long Covid, according to the most recent data from the U.S. Census Bureau’s Household Pulse Survey.
Dr. Monica Verduzco-Gutierrez, chair of rehabilitation medicine at the University of Texas Health Science Center at San Antonio and head of its long Covid clinic, praised the new study.
“Understanding the mechanisms of long Covid is how we’re going to figure out treatments,” she said.
Other studies have also identified potential mechanisms. In one study, published in the October issue of the journal Cell, researchers suggested that remnants of the virus lingering in the gut of long Covid patients triggered reductions in the neurotransmitter serotonin. Lower serotonin levels, they said, could explain some neurological and cognitive symptoms. Another study, published in the journal Nature in September by Iwasaki and her colleagues, found that long Covid patients had significantly lower levels of the hormone cortisol than other Covid patients and healthy controls. Cortisol helps people feel alert and awake.
Verduzco-Gutierrez, Iwasaki and Boyman agree that the new research points the way toward developing diagnostic tests and treatment by focusing on the proteins of the complement system.
However, Boyman and his colleagues used cutting-edge, complicated methods for detecting the differences in these proteins that could not be used in a routine diagnostic lab.
“We need companies already active in diagnostics that have sufficient manpower and financial power” to develop a simplified test, he said.
Once a test is developed, or with rigorous screening for long Covid patients, pharmaceutical companies could begin clinical trials of potential treatments, Boyman said. Drugs already exist to modulate and inhibit the complement system for very rare immune diseases that affect the kidneys, muscles or nervous system, and they could be tested in long Covid patients, he said.
New drugs could also be developed, Iwasaki said.
“I think there are a lot of things that we can try in the future,” she said. But first, the results of this study need to be replicated, as with any research, she added.
Verduzco-Gutierrez said she would like to see any future studies follow patients for a longer period of time. “What about people who have had long Covid for three years? We don’t know what their blood looks like,” she said.






