A German man has probably been cured of HIV, a medical milestone achieved by only six other people in the more than 40 years since the AIDS epidemic began.
The German man, who prefers to remain anonymous, was treated for acute myeloid leukemia, or AML, with a stem cell transplant in October 2015. He stopped taking his antiretroviral drugs in September 2018 and remains in viral remission with no rebound. Multiple ultra-sensitive tests have detected no viable HIV in his body.
In a statement, the man said of his remission: “A healthy person has many wishes, a sick person only one.”
The case, which investigators said offered vital lessons for HIV cure research, is expected to be presented Wednesday by Dr. Christian Gaebler, a physician-scientist at the Charité-Universitätsmedizin Berlin, at the 25th International AIDS Conference in Munich.
“The longer we see these HIV remissions without any HIV therapy, the more confidence we can get that we’re probably seeing a case where we really have eradicated all competent HIV,” Gaebler said.
As with all previous cases of potential HIV cure, experts are eager to temper public excitement with a caveat: The treatment that apparently thwarted the virus in the seven patients will ever be available to only a select few. All contracted HIV and later developed blood cancer, which demanded stem cell transplants to treat the malignancy.
The transplants — in most cases from donors selected because their immune cells, the cells that HIV targets — boasted a rare, natural resistance to the virus and were instrumental in apparently eradicating all viable, or competent, copies of the virus from the body.
Stem cell transplants are highly toxic and can be fatal. So it would be unethical to provide them to people with HIV except to treat separate diseases, like blood cancer.
HIV is monumentally difficult to cure because some of the cells it infects are long-living immune cells that are in or enter a dormant state. Standard antiretroviral treatment for HIV works only on immune cells that, typical of infected cells, are actively making new viral copies. Consequently, HIV within resting cells stays under the radar. Collectively, such cells are known as the viral reservoir.
At any moment, a reservoir cell can start producing HIV. That is why if people with the virus stop taking their antiretrovirals, their viral loads typically rebound within weeks.
A stem cell transplant has the potential to cure HIV in part because it requires destroying a person’s cancer-afflicted immune system with chemotherapy and sometimes radiation and replacing it with a donor’s healthy immune system.
In five of the seven cases of definite or possible HIV cure, doctors found donors who had rare, natural defects in both copies of a gene that gives rise to a particular protein, called CCR5, on the surface of immune cells. Most HIV strains attach to that protein to infect cells. Without functional CCR5 proteins, immune cells are HIV-resistant.
The German man’s donor had just one copy of the CCR5 gene, meaning his immune cells most likely have about half the normal quantity of that protein. In addition, he had only one copy of the gene himself. Together, those two genetic factors may have upped his chances of a cure, Gaebler said.
While having two copies of the defective CCR5 gene is rare, occurring in about 1% of people with native northern European ancestry, having one copy occurs in about 16% of such people.
“So the study suggests that we can broaden the donor pool for these kinds of cases,” Dr. Sharon Lewin, director of the Peter Doherty Institute for Infection and Immunity in Melbourne, Australia, said in a media briefing last week.
Interestingly, a man treated in Geneva whose possible HIV cure was announced last year had a donor with two normal copies of the CCR5 gene. So his transplanted immune cells were not HIV-resistant.
Those two recent European cases raise critical questions about the factors that actually contribute to a successful HIV cure.
“The level of protection one might have predicted from transplant should not have been enough to prevent the virus from surviving and rebounding,” Dr. Steven Deeks, a leading HIV cure researcher at the University of California, San Francisco, who is not involved with the German man’s care, said of his case. “There are several testable theories, so I am optimistic we will learn something here that could shape the next generation of cure studies.”
Gaebler said having HIV-resistant immune cells in the mix surely greatly improves the chances of success in curing the virus with a stem cell transplant. And yet, he said, lacking that safety net, or having one with some holes in it, as with the German man, does not preclude success.
“We need to understand how the new immune system successfully grafted into his body and how it successfully eliminated HIV reservoirs over time,” he said. Suggesting that the transplanted immune cells may have attacked the viral reservoir, he said, “The donor’s innate immune system might have played an important role here.”
The 6 others cured or possibly cured of HIV
All were initially known by pseudonyms based on where they were treated.
- Timothy Ray Brown, aka the “Berlin patient.” Brown, an American living in Germany, was treated for AML. When his case was announced in 2008, it galvanized the HIV research field. Born in 1966, he was cured of HIV but died of recurrent leukemia in 2020.

- Adam Castillejo, aka the “London patient.” Castillejo, 44, a Venezuelan man living in England, received a stem cell transplant for AML in 2016 and stopped HIV treatment in 2017. He is considered cured.
- Marc Franke, the “Düsseldorf patient.” Treated with a stem cell transplant for AML in 2013, Franke, 55, went off antiretrovirals in November 2018 and is considered cured.

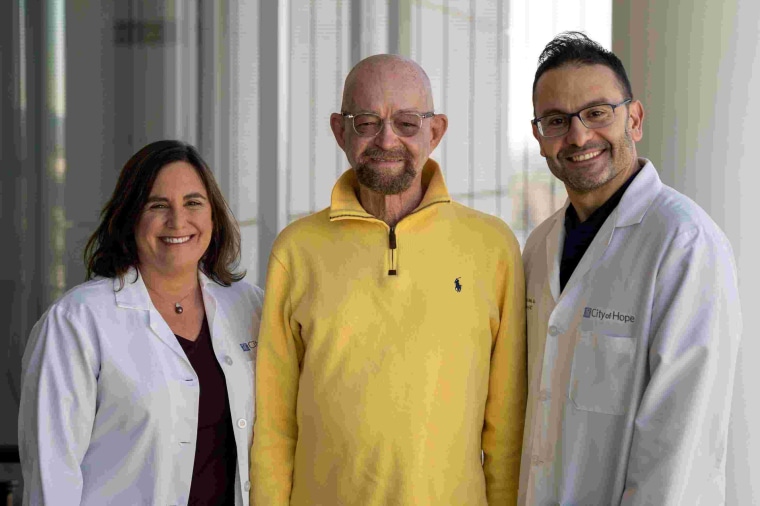
- Paul Edmonds, aka the “City of Hope patient.” Edmonds, the oldest potential cure case at 63 when he received a stem-cell transplant for AML in 2019, received reduced-intensity chemotherapy because of his age. Off antiretrovirals since March 2021, he will be considered cured when he hits five years with no viral rebound. In an interview, he expressed excitement over the new case of a man probably cured, as well, and said, “My vision is clear: a world where HIV is no longer a sentence, but a footnote in history.”
- The “New York patient.” The first woman and person of mixed-race ancestry possibly to be cured, she was diagnosed with leukemia in 2017 and received a stem cell transplant augmented with umbilical cord blood, which allowed for a lower genetic match with her donor, thus broadening the donor pool.
- The “Geneva patient.” In his 50s, he was diagnosed with a rare blood cancer in 2018 and has been off of HIV treatment since November 2021. Researchers remain cautious about his cure status because his immune cells are not HIV resistant.
Franke, Edmonds and Castillejo, who have become friends, are expected to attend the HIV conference in Munich.






